Acne vulgaris and its resulting scarring remain among the most prevalent dermatological conditions globally, often contributing to long-lasting physical and psychosocial impact. Traditional therapeutic approaches, while beneficial, may not adequately address both active lesions and the persistent scars that follow. In recent years, microneedling has emerged as a minimally invasive modality with increasing clinical interest. This article explores the scientific rationale, clinical efficacy, and practical considerations for microneedling in treating acne and acne-related scarring.
Mechanism of Action: Collagen Induction and Cutaneous Remodeling
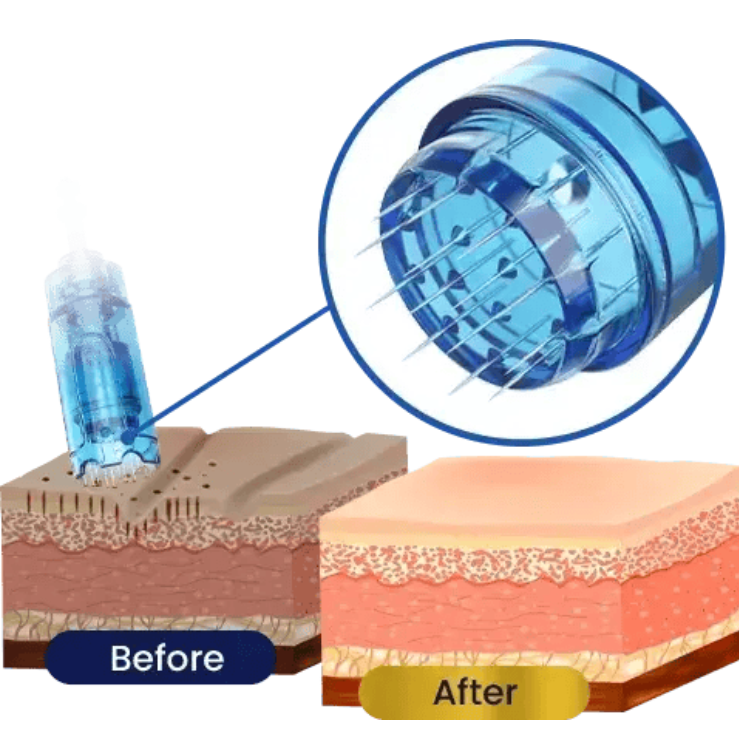
Microneedling, or percutaneous collagen induction therapy, involves using fine, sterile needles to create controlled micro-injuries in the skin. These micro-channels stimulate the body’s natural wound healing cascade, resulting in the release of growth factors and cytokines, including:
- Platelet-derived growth factor (PDGF)
- Transforming growth factor-beta (TGF-β)
- Fibroblast growth factor (FGF)
- Epidermal growth factor (EGF)
The regenerative cascade initiated by microneedling promotes neo-collagenesis and neo-elastogenesis, crucial for improving atrophic acne scars. Furthermore, these microchannels enhance the transdermal delivery of topicals such as hyaluronic acid, retinoids, and vitamin C, optimizing their therapeutic benefits. In cases of active acne, microneedling may also exert anti-inflammatory effects and reduce sebaceous gland activity when paired with adjunct modalities such as radiofrequency or light therapy.
Clinical Context: Acne and Acne Scarring
Acne is a chronic inflammatory condition of the pilosebaceous unit. Many patients respond to conventional therapies, including retinoids, antibiotics, and hormonal treatments; some experience persistent or recurrent lesions and scarring. Acne scars may present in various morphologies, including icepick, rolling, and boxcar types, and often prove resistant to topical therapies alone.
Scarring affects skin integrity and impairs quality of life. Therefore, an effective treatment must address both inflammation and structural dermal damage. Microneedling has been proposed as a therapeutic option capable of intervening across these phases.
Evidence-Based Review
Microneedling for Active Acne
A 2023 prospective clinical trial assessed the safety and efficacy of microneedling in patients with moderate to severe inflammatory and non-inflammatory acne. Subjects underwent three treatment sessions at four-week intervals. The results demonstrated a statistically significant reduction in both lesion counts and sebum excretion levels post-treatment. Notably, inflammatory lesions showed greater improvement than non-inflammatory lesions. Adverse events were limited to transient erythema and mild discomfort, resolving within 48 hours.
Another recent pilot study confirmed that microneedling did not exacerbate acne or disrupt the skin microbiome, dispelling prior concerns regarding its use in active acne. This represents a paradigm shift, positioning microneedling as a viable therapeutic option during active breakouts.
Microneedling for Acne Scarring
Multiple randomized controlled trials (RCTs) have established the role of microneedling in managing atrophic acne scars. A 2022 meta-analysis of twelve RCTs involving over 400 patients concluded that microneedling monotherapy significantly improved scar severity without increasing the risk of post-inflammatory hyperpigmentation, particularly in patients with darker skin types.
A 2023 split-face trial investigating the combined use of microneedling and platelet-rich plasma (PRP) found superior clinical outcomes compared to microneedling alone. The study reported greater scar depth and overall skin texture improvements in the combination therapy group, aligning with increased patient satisfaction.
In another study, researchers evaluated two PRP preparation methods combined with microneedling. Both approaches produced significant improvement in acne scarring, further supporting the efficacy of PRP as an adjunct in microneedling protocols.
The Role of FDA-Cleared Microneedling Devices
As microneedling gains traction in clinical dermatology and aesthetics, device safety and regulatory compliance become essential for practice integration. FDA-cleared microneedling pens have undergone review for safety and intended use, providing clinicians with confidence in device quality and patient outcomes. These systems often feature adjustable needle depths, consistent motor performance, and sterile, single-use cartridges, attributes critical for maintaining treatment efficacy while minimizing risk of infection or complications.
For medical professionals considering incorporating microneedling into their aesthetic or dermatologic protocols, FDA-cleared devices can ensure adherence to regulatory standards while optimizing therapeutic consistency. Such devices also support integration with regenerative adjuncts like exosomes, platelet-rich plasma, and bioactive topicals.
Treatment Protocols and Parameters
Protocols vary based on scar morphology, patient skin type, and adjunctive treatments. Standard microneedling sessions are performed every 4 to 6 weeks, with most protocols recommending 3 to 6 treatments for optimal results. Needle depth and speed can be customized to target different dermis layers. More superficial penetration may suffice for active acne, whereas deeper penetration is recommended for atrophic scars.
The following table outlines typical clinical approaches:
| Treatment Focus | Needle Depth | Frequency | Adjunct Modalities | Comments |
| Active Acne | 0.5–1.0 mm | Every 4 weeks | Topical retinoids, RF | Reduces inflammation and sebum |
| Atrophic Scarring | 1.5–2.5 mm | Monthly | PRP, Chemical Peels, Hyaluronic Acid | Enhances collagen production |
| Post-inflammatory Erythema | 0.5–1.0 mm | Bi-monthly | Light therapy | Aids in reducing vascular redness |
Safety Profile and Contraindications
Microneedling is generally well-tolerated. Common adverse effects include:
- Mild erythema
- Edema
- Pinpoint bleeding
- Skin tightness
These effects are transient and typically resolve within 24 to 72 hours. The average downtime is minimal, allowing patients to resume normal activities quickly.
Relative contraindications include:
- Active skin infections (e.g., herpes simplex)
- Keloid-prone individuals
- Use of isotretinoin within the last 6 months
- Uncontrolled diabetes or bleeding disorders
Proper skin preparation and post-treatment care, including gentle cleansing, emollients, and photoprotection, are essential to minimize risk and support recovery.
Clinical Implications
For medical professionals seeking safe, minimally invasive, and cost-effective options for acne management, microneedling offers robust versatility. It addresses inflammatory lesions and atrophic scars through mechanisms rooted in the skin’s regenerative biology. Its favorable safety profile and adaptability to various skin types make it particularly attractive in aesthetic and integrative practices.
Emerging innovations such as RF-enhanced microneedling and combination therapy with PRP or chemical agents continue to improve outcomes and patient satisfaction. When integrated thoughtfully into a treatment protocol and performed with FDA-cleared microneedling devices, this modality can enhance the effectiveness of an aesthetic or dermatologic practice.
Conclusion
Microneedling has developed into a scientifically validated intervention for acne and its sequelae. Backed by randomized controlled trials and mechanistic understanding, it bridges conventional dermatologic care and regenerative medicine. Its clinical utility spans active acne, acne scarring, and pigmentation disorders. With appropriate patient selection, technique, and equipment, microneedling offers a reliable and reproducible outcome that aligns with the goals of modern integrative dermatology.
References
- Alqam ML, Jones BC, Hitchcock TM. (2023). Study to determine the safety and efficacy of microneedling as an effective treatment for acne vulgaris. Skin Health and Disease, 3(5):e264. https://doi.org/10.1002/ski2.264
- Shen YC, Chiu WK, Kang YN, Chen C. (2022). Microneedling monotherapy for acne scar: systematic review and meta-analysis of randomized controlled trials. Aesthetic Plastic Surgery, 46(4):1913–1922. https://doi.org/10.1007/s00266-022-02845-3
- Shoaib ME, Alharthi SS, et al. (2023). Subcision with a blunt cannula in combination with injection of PRP and microneedling in the treatment of acne scars. The Egyptian Journal of Hospital Medicine, 90(1):2050–2055. https://doi.org/10.21608/ejhm.2023.291007
- Singh A, Yadav D, Kumari K, et al. (2024). Comparative study of the efficacy of PRP (Double Spin vs TD-TU Technique) with microneedling for atrophic acne scars. Medico-Legal Update, 8(4):10–15. https://doi.org/10.31674/mjmr.2024.v08i04.003
- Kang C, et al. (2022). Combined treatment with microneedling and platelet‑rich plasma is more effective than microneedling without PRP for patients with acne scars: meta‑analysis. Frontiers in Medicine, 8:788754. https://doi.org/10.3389/fmed.2021.788754
- Huang CC, Mao MP, Peng YR, et al. (2024). Efficacy and safety of single microneedle radiofrequency vs. photodynamic therapy on moderate‑to‑severe acne vulgaris: a prospective, randomized, controlled study. Chinese Medical Journal, 137(8):1006–1008. https://doi.org/10.1097/CM9.0000000000002911
- Niaz G, Ajeebi Y, Alshamrani H, Khalmurad M, Lee KC. (2025). Fractional Radiofrequency Microneedling as a Monotherapy in Acne Scar Management: A Systematic Review of Current Evidence. Clinical, Cosmetic and Investigational Dermatology, 18:19–29. https://doi.org/10.2147/ccid.s502295


